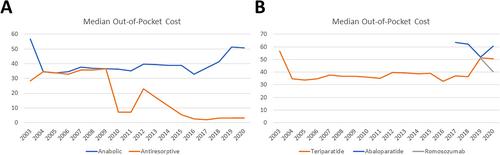
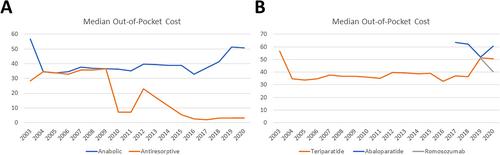
{"title":"Anabolic and Antiresorptive Osteoporosis Treatment: Trends, Costs, and Sequence in a Commercially Insured Population, 2003–2021","authors":"Harsh Wadhwa, Janet Y Wu, Jennifer S Lee, Corinna C Zygourakis","doi":"10.1002/jbm4.10800","DOIUrl":null,"url":null,"abstract":"<p>New anabolic medications (abaloparatide and romosozumab) were recently approved for osteoporosis, and data suggest that prescribing antiresorptive medications after a course of anabolic medications offers better outcomes. This study aimed to characterize prescription trends, demographics, geographical distributions, out-of-pocket costs, and treatment sequences for anabolic and antiresorptive osteoporosis medications. Using a commercial claims database (Clinformatics Data Mart), adult patients with osteoporosis from 2003 to 2021 were retrospectively reviewed and stratified based on osteoporosis medication class. Patient demographics and socioeconomic variables, provider types, and out-of-pocket costs were collected. Multivariable regression analyses were used to identify independent predictors of receiving osteoporosis treatment. A total of 2,988,826 patients with osteoporosis were identified; 616,635 (20.6%) received treatment. Patients who were female, Hispanic or Asian, in the Western US, had higher net worth, or had greater comorbidity burden were more likely to receive osteoporosis medications. Among patients who received medication, 31,112 (5.0%) received anabolic medication; these were more likely to be younger, White patients with higher education level, net worth, and greater comorbidity burden. Providers who prescribed the most anabolic medications were rheumatologists (18.5%), endocrinologists (16.8%), and general internists (15.3%). Osteoporosis medication prescriptions increased fourfold from 2003 to 2020, whereas anabolic medication prescriptions did not increase at this rate. Median out-of-pocket costs were $17 higher for anabolic than antiresorptive medications, though costs for anabolic medications decreased significantly from 2003 to 2020 (compound annual growth rate: −0.6%). A total of 8388 (1.4%) patients tried two or more osteoporosis medications, and 0.6% followed the optimal treatment sequence. Prescription of anabolic osteoporosis medications has not kept pace with overall osteoporosis treatment, and there are socioeconomic disparities in anabolic medication prescription, potentially driven by higher median out-of-pocket costs. Although prescribing antiresorptive medications after a course of anabolic medications offers better outcomes, this treatment sequence occurred in only 0.6% of the study cohort. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>","PeriodicalId":14611,"journal":{"name":"JBMR Plus","volume":"7 10","pages":""},"PeriodicalIF":3.4000,"publicationDate":"2023-07-24","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10800","citationCount":"1","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"JBMR Plus","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10800","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ENDOCRINOLOGY & METABOLISM","Score":null,"Total":0}
引用次数: 1
Abstract
New anabolic medications (abaloparatide and romosozumab) were recently approved for osteoporosis, and data suggest that prescribing antiresorptive medications after a course of anabolic medications offers better outcomes. This study aimed to characterize prescription trends, demographics, geographical distributions, out-of-pocket costs, and treatment sequences for anabolic and antiresorptive osteoporosis medications. Using a commercial claims database (Clinformatics Data Mart), adult patients with osteoporosis from 2003 to 2021 were retrospectively reviewed and stratified based on osteoporosis medication class. Patient demographics and socioeconomic variables, provider types, and out-of-pocket costs were collected. Multivariable regression analyses were used to identify independent predictors of receiving osteoporosis treatment. A total of 2,988,826 patients with osteoporosis were identified; 616,635 (20.6%) received treatment. Patients who were female, Hispanic or Asian, in the Western US, had higher net worth, or had greater comorbidity burden were more likely to receive osteoporosis medications. Among patients who received medication, 31,112 (5.0%) received anabolic medication; these were more likely to be younger, White patients with higher education level, net worth, and greater comorbidity burden. Providers who prescribed the most anabolic medications were rheumatologists (18.5%), endocrinologists (16.8%), and general internists (15.3%). Osteoporosis medication prescriptions increased fourfold from 2003 to 2020, whereas anabolic medication prescriptions did not increase at this rate. Median out-of-pocket costs were $17 higher for anabolic than antiresorptive medications, though costs for anabolic medications decreased significantly from 2003 to 2020 (compound annual growth rate: −0.6%). A total of 8388 (1.4%) patients tried two or more osteoporosis medications, and 0.6% followed the optimal treatment sequence. Prescription of anabolic osteoporosis medications has not kept pace with overall osteoporosis treatment, and there are socioeconomic disparities in anabolic medication prescription, potentially driven by higher median out-of-pocket costs. Although prescribing antiresorptive medications after a course of anabolic medications offers better outcomes, this treatment sequence occurred in only 0.6% of the study cohort. © 2023 The Authors. JBMR Plus published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.