Drinking alcohol may cause harm to an individual's health and social relationships, while a drinking culture may harm societies as it may increase crime rates and make an area feel less safe. Local councils in Greater Manchester, UK, developed the Communities in Charge of Alcohol (CICA) intervention, in which volunteers were trained to give alcohol-related advice to the public and taught how to influence policies to restrict when, where and how alcohol is sold. As part of a larger study, the aim of the current project is to measure the impact of CICA on health and crime outcomes at the lower super output (LSOA) geographical aggregation.
Quantitative evaluation using four time series analytic methods (stepped-wedge design, and comparisons to local controls, national controls and synthetic controls) with findings triangulated across these methods. A cost–benefit analysis was carried out alongside the effectiveness analysis.
The general public in Greater Manchester, UK, between 2010 and 2020.
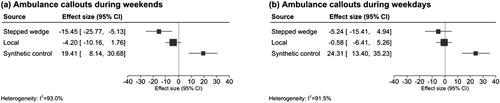
The primary outcome of interest was alcohol-related hospital admissions. Secondary outcomes were accident and emergency (A&E) attendances, ambulance callouts, recorded crimes and anti-social behaviour incidents.
Triangulation of the results did not indicate any consistent effect on area-level alcohol-related hospital admissions, A&E attendances, ambulance callouts, reported crimes or anti-social behaviour associated with the implementation of CICA. The primary stepped-wedge analysis indicated an increase in alcohol-related hospital admissions following the implementation of CICA of 13.4% (95% confidence interval −3.3%, +30.1%), which was consistent with analyses based on other methods with point estimates ranging from +3.4% to 16.4%.
There is no evidence of a measurable impact of the Communities in Charge of Alcohol (CICA) programme on area-level health and crime outcomes in Greater Manchester, UK, within 3 years of the programme start. The increase in alcohol-related hospital admissions was likely the result of other temporal trends rather than the CICA programme. Possible explanations include insufficient follow-up time, too few volunteers trained, volunteers being unwilling to get involved in licensing decisions or that the intervention has no direct impact on the selected outcomes.