{"title":"Hypervitaminosis D Secondary to a CYP24A1 Loss-of-Function Mutation: An Unusual Cause of Hypercalcemia in Two Siblings","authors":"Lucy Collins, Emma Boehm, Catherine Luxford, Roderick Clifton-Bligh, Vivian Grill","doi":"10.1002/jbm4.10788","DOIUrl":null,"url":null,"abstract":"<p>Hypervitaminosis D as a cause of hypercalcemia may be due to vitamin D intoxication, granulomatous diseases, or abnormalities of vitamin D metabolism. The <i>CYP24A1</i> gene encodes for the 24-hydroxylase enzyme, which is responsible for the catabolism of 25-hydroxyvitamin D (25(OH)D) and 1,25-dihydroxyvitamin D (1,25(OH)2D). Mutations in <i>CYP24A1</i> can result in elevated 1,25(OH)2D causing parathyroid hormone (PTH)-independent hypercalcemia, hypercalciuria, nephrolithiasis, and nephrocalcinosis. We present the cases of two siblings exhibiting hypercalcemia secondary to a <i>CYP24A1</i> loss-of-function mutation. Case 1 presented initially with PTH-dependent hypercalcemia, with localization of a left upper parathyroid adenoma on parathyroid technetium sestamibi (<sup>99m</sup>Tc-MIBI) uptake study. Despite parathyroidectomy (180 mg adenoma), hypercalcemia, hypercalciuria, and low normal PTH levels persisted. A repeat parathyroid <sup>99m</sup>Tc-MIBI uptake study localized a second adenoma and a right inferior parathyroidectomy was performed (170 mg adenoma). PTH subsequently became undetectable, however hypercalcemia and hypercalciuria persisted. A new presentation of PTH-independent hypercalcemia found to be secondary to a <i>CYP24A1</i> loss-of-function mutation in his sibling, Case 2, signaled the underlying cause. Cascade testing confirmed both siblings were homozygous for the pathogenic variant c.1186C>T, p.Arg396Trp (R396W) of <i>CYP24A1</i> (NM_000782.5). In clinical practice <i>CYP24A1</i> loss-of-function mutations should be considered in patients presenting with PTH-independent hypercalcemia, hypercalciuria, and 1,25(OH)2D levels in the upper normal or elevated range. Although in our case assays of 24,25(OH)2D were not available, calculation of the 25(OH)D:24,25(OH)2D ratio can assist in the diagnostic process. Possible treatments to manage the risk of hypercalcemia in patients with a <i>CYP24A1</i> loss-of-function mutation include avoidance of vitamin D oversupplementation and excessive sun exposure. Hydration and bisphosphonate therapy can be useful in managing the hypercalcemia. Although not utilized in our cases, treatment with ketoconazole, fluconazole, and rifampicin have been described as potential therapeutic options. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>","PeriodicalId":14611,"journal":{"name":"JBMR Plus","volume":"7 9","pages":""},"PeriodicalIF":2.4000,"publicationDate":"2023-08-08","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10788","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"JBMR Plus","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10788","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ENDOCRINOLOGY & METABOLISM","Score":null,"Total":0}
引用次数: 0
Abstract
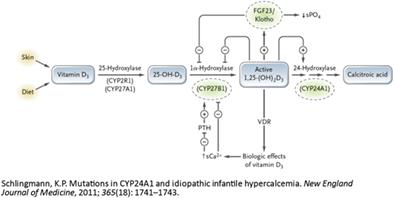
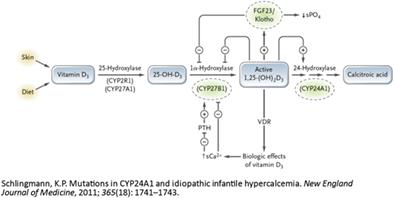
Hypervitaminosis D as a cause of hypercalcemia may be due to vitamin D intoxication, granulomatous diseases, or abnormalities of vitamin D metabolism. The CYP24A1 gene encodes for the 24-hydroxylase enzyme, which is responsible for the catabolism of 25-hydroxyvitamin D (25(OH)D) and 1,25-dihydroxyvitamin D (1,25(OH)2D). Mutations in CYP24A1 can result in elevated 1,25(OH)2D causing parathyroid hormone (PTH)-independent hypercalcemia, hypercalciuria, nephrolithiasis, and nephrocalcinosis. We present the cases of two siblings exhibiting hypercalcemia secondary to a CYP24A1 loss-of-function mutation. Case 1 presented initially with PTH-dependent hypercalcemia, with localization of a left upper parathyroid adenoma on parathyroid technetium sestamibi (99mTc-MIBI) uptake study. Despite parathyroidectomy (180 mg adenoma), hypercalcemia, hypercalciuria, and low normal PTH levels persisted. A repeat parathyroid 99mTc-MIBI uptake study localized a second adenoma and a right inferior parathyroidectomy was performed (170 mg adenoma). PTH subsequently became undetectable, however hypercalcemia and hypercalciuria persisted. A new presentation of PTH-independent hypercalcemia found to be secondary to a CYP24A1 loss-of-function mutation in his sibling, Case 2, signaled the underlying cause. Cascade testing confirmed both siblings were homozygous for the pathogenic variant c.1186C>T, p.Arg396Trp (R396W) of CYP24A1 (NM_000782.5). In clinical practice CYP24A1 loss-of-function mutations should be considered in patients presenting with PTH-independent hypercalcemia, hypercalciuria, and 1,25(OH)2D levels in the upper normal or elevated range. Although in our case assays of 24,25(OH)2D were not available, calculation of the 25(OH)D:24,25(OH)2D ratio can assist in the diagnostic process. Possible treatments to manage the risk of hypercalcemia in patients with a CYP24A1 loss-of-function mutation include avoidance of vitamin D oversupplementation and excessive sun exposure. Hydration and bisphosphonate therapy can be useful in managing the hypercalcemia. Although not utilized in our cases, treatment with ketoconazole, fluconazole, and rifampicin have been described as potential therapeutic options. © 2023 The Authors. JBMR Plus published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.
CYP24A1功能缺失突变引起的维生素D过多:两个兄弟姐妹高钙血症的异常原因
维生素D过多是导致高钙血症的原因,可能是由于维生素D中毒、肉芽肿性疾病或维生素D代谢异常。CYP24A1基因编码24-羟化酶,该酶负责25-羟基维生素D(25(OH)D)和1,25-二羟基维生素D的分解代谢。CYP24A1的突变可导致1,25(OH)2D升高,导致甲状旁腺激素(PTH)非依赖性高钙血症、高钙尿症、肾结石和肾钙沉着症。我们报告了两个兄弟姐妹因CYP24A1功能缺失突变而出现高钙血症的病例。病例1最初表现为甲状旁腺激素依赖性高钙血症,在甲状旁腺锝-倍他米比(99mTc-MIBI)摄取研究中定位为左上甲状旁腺腺瘤。尽管进行了甲状旁腺切除术(180 mg腺瘤)、高钙血症、高钙尿和低正常PTH水平持续存在。一项重复的甲状旁腺99mTc-MIBI摄取研究定位了第二个腺瘤,并进行了右下甲状旁腺切除术(170 mg腺瘤)。PTH随后检测不到,但高钙血症和高钙尿持续存在。一种新的PTH非依赖性高钙血症的表现被发现是继发于他的兄弟姐妹CYP24A1功能缺失突变,病例2,这表明了潜在的原因。级联测试证实两个兄弟姐妹对于致病性变体c.1186C>;T、 p.CYP24A1(NM_000782.5)的Arg396Trp(R396W)。在临床实践中,在PTH非依赖性高钙血症、高钙尿症和1,25(OH)2D水平处于正常上限或升高范围的患者中,应考虑CYP24A1功能缺失突变。尽管在我们的病例中,24,25(OH)2D的测定不可用,但计算25(OH:D:24,25(OH2D)比率可以帮助诊断过程。CYP24A1功能丧失突变患者患高钙血症风险的可能治疗方法包括避免维生素D供应过剩和过度暴露在阳光下。水合和双磷酸盐治疗可用于治疗高钙血症。尽管在我们的病例中没有使用,但酮康唑、氟康唑和利福平的治疗已被描述为潜在的治疗选择。©2023作者。由Wiley Periodicals LLC代表美国骨与矿物研究学会出版的JBMR Plus。
本文章由计算机程序翻译,如有差异,请以英文原文为准。