We sought to collect granular data on temperature burden to further explore existing conflicting information on the relationship between temperature alterations and outcomes in patients with sepsis requiring hospital admission.
This was a prospective cohort study that enrolled a convenience sample of patients with sepsis or septic shock admitted to the hospital from the emergency department (ED). A “unit of temperature burden (UTB)” was defined as >1°C (1.8°F) above or below 37°C (98.6°F) for 1 min. Fever burden was defined as the number of UTBs >38°C (100.4°F). The primary objective was to calculate the fever burden in patients with sepsis during their ED stay. This was analyzed for patients who present to triage febrile or hypothermic and also for those who developed temperature abnormalities during their ED stay. The secondary objectives were correlating fever and hypothermia burden with in-hospital mortality, Systemic Inflammatory Response Syndrome (SIRS) criteria, and the quick Sequential (Sepsis-Associated) Organ Failure Assessment (qSOFA) score and identification of patients who may benefit from early implementation of targeted temperature management.
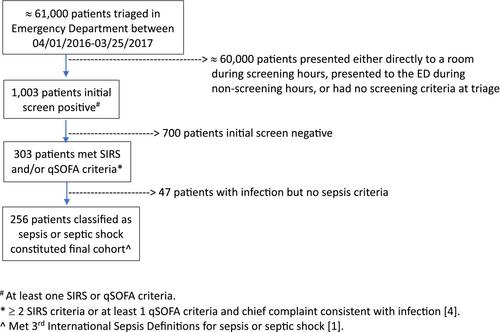
A total of 256 patients met the inclusion criteria. The mean age of patients was 60.1 ± 18.4 years; 46% were female and 29.6% were black. The median (interquartile range [IQR]) fever burden for the fever in triage cohort (n = 99) was 364.6 (174.3-716.8) UTB and for the no fever in triage cohort (n = 157) was 179.3 (80.9-374.0) UTB (p = 0.005). The two groups had similar in-hospital mortality (6.1 vs 8.3%; p = 0.5). The median fever burden for the fever anytime cohort was 303.8 (IQR 138.8-607.9) UTB and they had lower mortality than the no fever anytime cohort (4.7% vs 11.2%; p = 0.052). Patients with fever at triage had higher mean SIRS criteria than those without (2.8 vs 2.0; p < 0.001) while qSOFA points were similar (p = 0.199). A total of 27 patients had hypothermia during their ED stay and these patients were older with higher mean SIRS criteria.
Patients with sepsis and septic shock have a significant temperature burden in the ED. When comparing patients who had fever at any time during their ED stay with those who never had a fever, a trend toward an inverse relationship between fever burden and mortality was found.