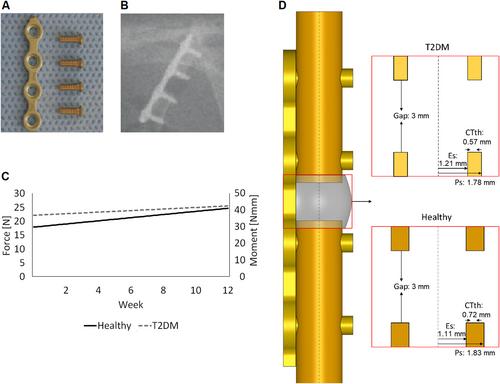
{"title":"基质细胞和成骨细胞功能受损导致2型糖尿病大鼠骨再生减少——计算机模型研究","authors":"Mahdi Jaber, Lorenz C Hofbauer, Christine Hofbauer, Georg N Duda, Sara Checa","doi":"10.1002/jbm4.10809","DOIUrl":null,"url":null,"abstract":"<p>Bone has the fascinating ability to self-regenerate. However, under certain conditions, such as type 2 diabetes mellitus (T2DM), this ability is impaired. T2DM is a chronic metabolic disease known by the presence of elevated blood glucose levels that is associated with reduced bone regeneration capability, high fracture risk, and eventual non-union risk after a fracture. Several mechanical and biological factors relevant to bone regeneration have been shown to be affected in a diabetic environment. However, whether impaired bone regeneration in T2DM can be explained due to mechanical or biological alterations remains unknown. To elucidate the relevance of either one, the aim of this study was to investigate the relative contribution of T2DM-related alterations on either cellular activity or mechanical stimuli driving bone regeneration. A previously validated in silico computer modeling approach that was capable of explaining bone regeneration in uneventful conditions of healing was further developed to investigate bone regeneration in T2DM. Aspects analyzed included the presence of mesenchymal stromal cells (MSCs), cellular migration, proliferation, differentiation, apoptosis, and cellular mechanosensitivity. To further verify the computer model findings against in vivo data, an experimental setup was replicated, in which regeneration was compared in healthy and diabetic after a rat femur bone osteotomy stabilized with plate fixation. We found that mechanical alterations had little effect on the reduced bone regeneration in T2DM and that alterations in MSC proliferation, MSC migration, and osteoblast differentiation had the highest effect. In silico predictions of regenerated bone in T2DM matched qualitatively and quantitatively those from ex vivo μCT at 12 weeks post-surgery when reduced cellular activities reported in previous in vitro and in vivo studies were included in the model. The presented findings here could have clinical implications in the treatment of bone fractures in patients with T2DM. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>","PeriodicalId":14611,"journal":{"name":"JBMR Plus","volume":"7 11","pages":""},"PeriodicalIF":3.4000,"publicationDate":"2023-10-02","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10809","citationCount":"0","resultStr":"{\"title\":\"Reduced Bone Regeneration in Rats With Type 2 Diabetes Mellitus as a Result of Impaired Stromal Cell and Osteoblast Function—A Computer Modeling Study\",\"authors\":\"Mahdi Jaber, Lorenz C Hofbauer, Christine Hofbauer, Georg N Duda, Sara Checa\",\"doi\":\"10.1002/jbm4.10809\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<p>Bone has the fascinating ability to self-regenerate. However, under certain conditions, such as type 2 diabetes mellitus (T2DM), this ability is impaired. T2DM is a chronic metabolic disease known by the presence of elevated blood glucose levels that is associated with reduced bone regeneration capability, high fracture risk, and eventual non-union risk after a fracture. Several mechanical and biological factors relevant to bone regeneration have been shown to be affected in a diabetic environment. However, whether impaired bone regeneration in T2DM can be explained due to mechanical or biological alterations remains unknown. To elucidate the relevance of either one, the aim of this study was to investigate the relative contribution of T2DM-related alterations on either cellular activity or mechanical stimuli driving bone regeneration. A previously validated in silico computer modeling approach that was capable of explaining bone regeneration in uneventful conditions of healing was further developed to investigate bone regeneration in T2DM. Aspects analyzed included the presence of mesenchymal stromal cells (MSCs), cellular migration, proliferation, differentiation, apoptosis, and cellular mechanosensitivity. To further verify the computer model findings against in vivo data, an experimental setup was replicated, in which regeneration was compared in healthy and diabetic after a rat femur bone osteotomy stabilized with plate fixation. We found that mechanical alterations had little effect on the reduced bone regeneration in T2DM and that alterations in MSC proliferation, MSC migration, and osteoblast differentiation had the highest effect. In silico predictions of regenerated bone in T2DM matched qualitatively and quantitatively those from ex vivo μCT at 12 weeks post-surgery when reduced cellular activities reported in previous in vitro and in vivo studies were included in the model. The presented findings here could have clinical implications in the treatment of bone fractures in patients with T2DM. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>\",\"PeriodicalId\":14611,\"journal\":{\"name\":\"JBMR Plus\",\"volume\":\"7 11\",\"pages\":\"\"},\"PeriodicalIF\":3.4000,\"publicationDate\":\"2023-10-02\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10809\",\"citationCount\":\"0\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"JBMR Plus\",\"FirstCategoryId\":\"1085\",\"ListUrlMain\":\"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10809\",\"RegionNum\":0,\"RegionCategory\":null,\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"Q2\",\"JCRName\":\"ENDOCRINOLOGY & METABOLISM\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"JBMR Plus","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10809","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ENDOCRINOLOGY & METABOLISM","Score":null,"Total":0}
引用次数: 0