{"title":"Changes in Vertebral Bone Density and Paraspinal Muscle Morphology Following Spaceflight and 1 Year Readaptation on Earth","authors":"Jennifer C. Coulombe, Fjola Johannesdottir, Katelyn A. Burkhart, Henriette Brummer, Brett T. Allaire, Mary L. Bouxsein","doi":"10.1002/jbm4.10810","DOIUrl":null,"url":null,"abstract":"<p>Astronauts have an increased risk of back pain and disc herniation upon returning to Earth. Thus, it is imperative to understand the effects of spaceflight and readaptation to gravity on the musculoskeletal tissues of the spine. Here we investigated whether ~6 months of spaceflight led to regional differences in bone loss within the vertebral body. Additionally, we evaluated the relationships between vertebral bone density and paraspinal muscle morphology before flight, after flight, and after readaptation on Earth. We measured vertebral trabecular bone mineral density (Tb.BMD), paraspinal muscle cross-sectional area (CSA), and muscle density in 17 astronauts using computed tomography (CT) images of the lumbar spine obtained before flight (before flight, <i>n</i> = 17), after flight (spaceflight, <i>n</i> = 17), and ~12 months of readaptation to gravitational loading on Earth (follow-up, <i>n</i> = 15). Spaceflight-induced declines in Tb.BMD were greater in the superior region of the vertebral body (−6.7%) than the inferior (−3.1%, <i>p</i> = 0.052 versus superior region) and transverse regions (−4.3%, <i>p</i> = 0.057 versus superior region). After a year of readaptation to Earth's gravity, Tb.BMD in the transverse region remained significantly below preflight levels (−4.66%, <i>p</i> = 0.0094). Paraspinal muscle CSA and muscle density declined −1.0% (<i>p</i> = 0.005) and −0.83% (<i>p</i> = 0.001) per month of spaceflight, respectively. Ultimately, bone loss in the superior vertebral body, along with fatty infiltration of paraspinal muscles and incomplete recovery even after a year of readaptation on Earth, may contribute to spinal pathology in long-duration astronauts. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>","PeriodicalId":14611,"journal":{"name":"JBMR Plus","volume":"7 12","pages":""},"PeriodicalIF":3.4000,"publicationDate":"2023-11-08","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10810","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"JBMR Plus","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10810","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ENDOCRINOLOGY & METABOLISM","Score":null,"Total":0}
引用次数: 0
Abstract
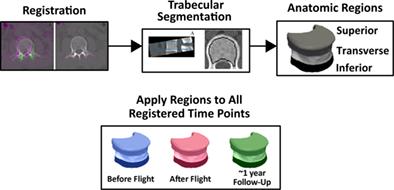
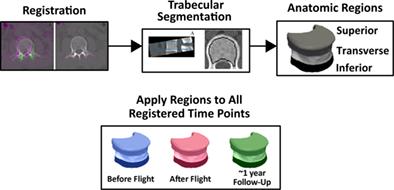
Astronauts have an increased risk of back pain and disc herniation upon returning to Earth. Thus, it is imperative to understand the effects of spaceflight and readaptation to gravity on the musculoskeletal tissues of the spine. Here we investigated whether ~6 months of spaceflight led to regional differences in bone loss within the vertebral body. Additionally, we evaluated the relationships between vertebral bone density and paraspinal muscle morphology before flight, after flight, and after readaptation on Earth. We measured vertebral trabecular bone mineral density (Tb.BMD), paraspinal muscle cross-sectional area (CSA), and muscle density in 17 astronauts using computed tomography (CT) images of the lumbar spine obtained before flight (before flight, n = 17), after flight (spaceflight, n = 17), and ~12 months of readaptation to gravitational loading on Earth (follow-up, n = 15). Spaceflight-induced declines in Tb.BMD were greater in the superior region of the vertebral body (−6.7%) than the inferior (−3.1%, p = 0.052 versus superior region) and transverse regions (−4.3%, p = 0.057 versus superior region). After a year of readaptation to Earth's gravity, Tb.BMD in the transverse region remained significantly below preflight levels (−4.66%, p = 0.0094). Paraspinal muscle CSA and muscle density declined −1.0% (p = 0.005) and −0.83% (p = 0.001) per month of spaceflight, respectively. Ultimately, bone loss in the superior vertebral body, along with fatty infiltration of paraspinal muscles and incomplete recovery even after a year of readaptation on Earth, may contribute to spinal pathology in long-duration astronauts. © 2023 The Authors. JBMR Plus published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.
太空飞行和在地球上重新适应 1 年后脊椎骨密度和脊柱旁肌肉形态的变化
宇航员返回地球后患背痛和椎间盘突出症的风险会增加。因此,了解太空飞行和重新适应重力对脊柱肌肉骨骼组织的影响势在必行。在此,我们研究了约 6 个月的太空飞行是否会导致椎体内骨质流失的区域性差异。此外,我们还评估了飞行前、飞行后和在地球上重新适应后脊椎骨密度与脊柱旁肌肉形态之间的关系。我们使用飞行前(飞行前,n = 17)、飞行后(太空飞行,n = 17)和在地球上重新适应重力负荷约 12 个月后(随访,n = 15)获得的腰椎计算机断层扫描(CT)图像,测量了 17 名宇航员的椎体骨小梁骨矿物质密度(Tb.BMD)、脊柱旁肌肉横截面积(CSA)和肌肉密度。太空飞行引起的椎体上部 Tb.BMD 下降率(-6.7%)大于下部(-3.1%,与上部相比 p = 0.052)和横向区域(-4.3%,与上部相比 p = 0.057)。在重新适应地球重力一年后,横向区域的 Tb.BMD 仍明显低于飞行前水平(-4.66%,p = 0.0094)。每飞行一个月,脊柱旁肌肉CSA和肌肉密度分别下降-1.0%(p = 0.005)和-0.83%(p = 0.001)。最终,椎体上部的骨质流失,加上脊柱旁肌肉的脂肪浸润以及在地球上重新适应一年后仍未完全恢复,可能会导致长期宇航员的脊柱病变。© 2023 作者。JBMR Plus 由 Wiley Periodicals LLC 代表美国骨矿研究学会出版。
本文章由计算机程序翻译,如有差异,请以英文原文为准。