Peri-operative neurocognitive disorders are one of the most common complications affecting older adults after anaesthesia and surgery. It is not clear how exposure to surgery and anaesthesia contributes to the prevalence of long-term neurocognitive disorders. This study aimed to report the prevalence of neurocognitive disorders, and explore pre-operative factors associated with neurocognitive disorders 5 years after elective orthopaedic surgery.
A prospective, 5-year longitudinal, cohort study was performed recruiting patients (aged ≥ 60 y) undergoing elective orthopaedic surgery and a contemporaneous non-surgical control group. Neurocognitive disorder was evaluated and classified at baseline and 5-year review incorporating: self- and informant-reported cognition; functional participation; and performance on neuropsychological tests.
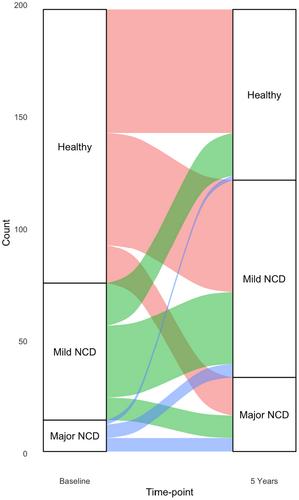
Recruitment at 5-year follow-up included 195 patients and 21 control participants. In the patient cohort the prevalence of neurocognitive disorder was 38.1% (n = 75), with 61 (30.1%) meeting the criteria for mild neurocognitive disorder and 14 (7.1%) for major neurocognitive disorder. At 5-year follow-up, 121 (61.4%) patients were classified with a neurocognitive disorder, with 88 (44.7%) characterised with mild neurocognitive disorder and 33 (16.8%) with major neurocognitive disorder. Age (odds ratio (95%CI) 1.07 (1.02–1.13); p = 0.01) and baseline cognitive impairment (odds ratio (95%CI) 2.1 (1.06–4.15); p = 0.03) were significant predictors of neurocognitive disorder 5 years after surgery.
More than half of older adult patients had some form of neurocognitive disorder 5 years after elective orthopaedic surgery. Surgery and anaesthesia may be associated with the trajectory of cognitive decline in at-risk older adults, including those with pre-operative cognitive impairment. Cognitive screening should be factored into pre-operative assessments of older adults to inform subsequent care.