There is increasing evidence that myosteatosis, which is currently not assessed in clinical routine, plays an important role in risk estimation in individuals with impaired glucose metabolism, as it is associated with the progression of insulin resistance. With advances in artificial intelligence, automated and accurate algorithms have become feasible to fill this gap.
In this retrospective study, we developed and tested a fully automated deep learning model using data from two prospective cohort studies (German National Cohort [NAKO] and Cooperative Health Research in the Region of Augsburg [KORA]) to quantify myosteatosis on whole-body T1-weighted Dixon magnetic resonance imaging as (1) intramuscular adipose tissue (IMAT; the current standard) and (2) quantitative skeletal muscle (SM) fat fraction (SMFF). Subsequently, we investigated the two measures for their discrimination of and association with impaired glucose metabolism beyond baseline demographics (age, sex and body mass index [BMI]) and cardiometabolic risk factors (lipid panel, systolic blood pressure, smoking status and alcohol consumption) in asymptomatic individuals from the KORA study. Impaired glucose metabolism was defined as impaired fasting glucose or impaired glucose tolerance (140–200 mg/dL) or prevalent diabetes mellitus.
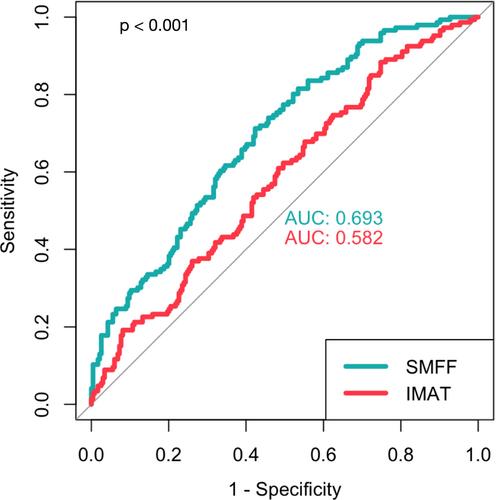
Model performance was high, with Dice coefficients of ≥0.81 for IMAT and ≥0.91 for SM in the internal (NAKO) and external (KORA) testing sets. In the target population (380 KORA participants: mean age of 53.6 ± 9.2 years, BMI of 28.2 ± 4.9 kg/m2, 57.4% male), individuals with impaired glucose metabolism (n = 146; 38.4%) were older and more likely men and showed a higher cardiometabolic risk profile, higher IMAT (4.5 ± 2.2% vs. 3.9 ± 1.7%) and higher SMFF (22.0 ± 4.7% vs. 18.9 ± 3.9%) compared to normoglycaemic controls (all P ≤ 0.005). SMFF showed better discrimination for impaired glucose metabolism than IMAT (area under the receiver operating characteristic curve [AUC] 0.693 vs. 0.582, 95% confidence interval [CI] [0.06–0.16]; P < 0.001) but was not significantly different from BMI (AUC 0.733 vs. 0.693, 95% CI [−0.09 to 0.01]; P = 0.15). In univariable logistic regression, IMAT (odds ratio [OR] = 1.18, 95% CI [1.06–1.32]; P = 0.004) and SMFF (OR = 1.19, 95% CI [1.13–1.26]; P < 0.001) were associated with a higher risk of impaired glucose metabolism. This signal remained robust after multivariable adjustment for baseline demographics and cardiometabolic risk factors for SMFF (OR = 1.10, 95% CI [1.01–1.19]; P = 0.028) but not for IMAT (OR = 1.14, 95% CI [0.97–1.33]; P = 0.11).
Quantitative SMFF, but not IMAT, is an independent predictor of impaired glucose metabolism, and discrimination is not significantly different from BMI, making it a promising alternative for the currently established approach. Automated methods such as the proposed model may provide a feasible option for opportunistic screening of myosteatosis and, thus, a low-cost personalized risk assessment solution.