Alcohol use disorder (AUD) with chronic and heavy alcohol consumption causes alcohol-associated liver disease (ALD). Early-stage ALD exhibits dyshomeostasis of zinc. We investigated the role of zinc deficiency in gut-barrier dysfunction, proinflammatory response, hepatocyte injury, and death, as well as potential sex differences in AUD patients.
Thirty-nine male and female AUD patients were grouped by normal [≥71 μg/dL (Group 1, number (n) = 26)] and low [<71 μg/dL (Group 2, n = 13)] serum zinc levels. Demographics, alcohol intake markers [Lifetime Drinking History (LTDH), heavy drinking days in the past 90-days (HDD90), total drinks in the past 90-days (TD90), number of drinking days in the past 90-days (NDD90), average drinks per day in the past 90 days (AvgDPD90)] were collected. Blood samples were tested for complete blood count (CBC), comprehensive metabolic panel (CMP), coagulation markers, gut-barrier dysfunction markers, cytokines, and hepatocyte death markers.
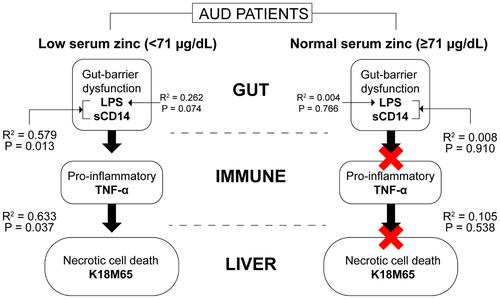
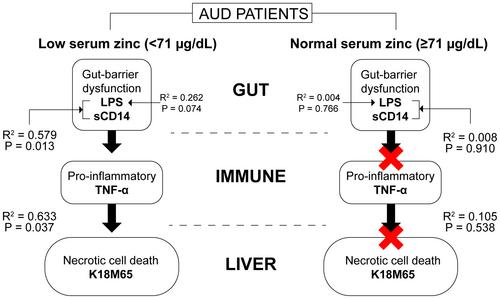
Group 2 females exhibited lower LTDH than Group 2 males (p = 0.028), but higher recent drinking. Aspartate transaminase: alanine transaminase (AST:ALT) ratio was higher (p = 0.049) in Group 2 males compared to Group 1 males. Overall, Group 2 showed threefold higher interleukin 8 (IL-8) levels than Group 1 (p = 0.92); these were sevenfold higher in Group 2 females than Group 1 females. Group 2 females also had higher K18M65, but lower K18M30 than Group 1 females. Necrotic type of cell death (K18M65) was well-described only in Group 2 by the arrangement of lipopolysaccharide (LPS), soluble cluster of differentiation 14 (sCD14), and tumor necrosis factor alpha (TNF-α) (R2 = 0.633, p = 0.037).
Our findings demonstrated the role of the gut-immune-liver axis in describing hepatocyte injury and death in zinc-deficient AUD patients. These patients represented an arrangement of gut-barrier dysfunction and an exacerbated immune response. Shift in the cell-death mechanism from apoptosis in zinc-replete females to necrosis in zinc-deficient females suggests a subclinical to clinical transition of ALD associated with zinc status.