The objective of this study is to examine the epidemiological characteristics of very elderly patients (aged over 80 years) with cancer admitted to the intensive care unit (ICU), and to elucidate the association between Acute Physiology Score III (APS-III) and 28-day mortality.
A retrospective analysis was conducted using data extracted from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database. Patients aged 80 years and above were assigned to three groups: non-cancer group, non-metastatic cancer group, and metastatic cancer group, based on their cancer diagnosis and its extent, Kaplan–Meier curves were constructed among these patient groups. Furthermore, patients were divided into a survival group and a non-survival group based on their 28-day survival status after ICU admission. Univariate and multivariate logistic regression analyses were performed to detect the risk factors for 28-day mortality among these patients. Additionally, this investigation sought to establish a dose–response relationship by exploring the graded association between APS-III scores and the 28-day mortalities among patients diagnosed with cancer.
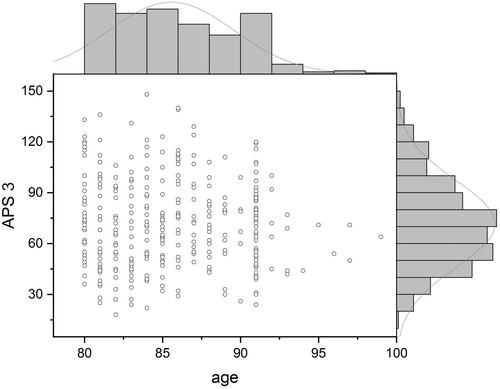
A total of 42,037 medical records were screened, from which 11,461 elderly patients aged over 80 years were included, comprising 1020 (8.90%) with non-metastatic cancer, 537 (4.68%) with metastatic cancer, and 9904 (86.41%) without cancer. Significant differences in 28-day mortality were observed between both the non-metastatic and metastatic cancer groups compared to the non-cancer group (20.98% and 22.35% vs. 15.75%, p < 0.001). However, no statistically significant difference was detected in the 28-day mortality rate when comparing the non-metastatic cancer group directly with the metastatic cancer group (20.98% vs. 22.35%, p = 0.576). Univariate analysis revealed significant differences (p < 0.001) in age, gender, BMI, aCCI excluding cancer point, ventilation, presence of cancer, and status of metastatic cancer between the survival and non-survival groups. In the multivariate logistic regression, the odds ratio (OR) for ventilation was found to be 2.154 (95% CI: 1.799–2.578), cancer conferred an OR of 1.499 (95% CI: 1.137–1.975), metastatic cancer showed an OR of 1.171 (95% CI: 0.745–1.841), APS-III showed an OR of 1.038 (95% CI: 1.034–1.042). A dose–response relationship was observed, demonstrating that when the APS-III score exceeded 80 points, the 28-day mortality rate surpassed 50% among the very elderly cancer patients in ICU.
More than one-tenth of critically ill very elderly patients admitted to the ICU are diagnosed with cancer. Among ICU patients, those with cancer face a short-term mortality risk approximately 1.5 times higher than those without a cancer diagnosis. Interestingly, while our findings do not indicate an escalated mortality risk due to metastasis within the cancer patient cohort, the presence of cancer itself remains a significant factor influencing ICU mortality rates in this very elderly population.