Evidence suggesting the benefits of compassionate, person-centred care, for both patients and physicians is accruing. Medical selection, for example, aims to choose future health professionals that possess the correct attitudes, beliefs and personal attributes to deliver such care. Moreover, once in training, these desirable personal qualities should be developed and maintained, sometimes in the face of adverse health care service conditions. However, advances in selecting for, and developing, these abilities and attributes in health care have been hindered by a lack of clarity regarding how the relevant skills and traits should be defined, measured, developed and maintained in clinicians.
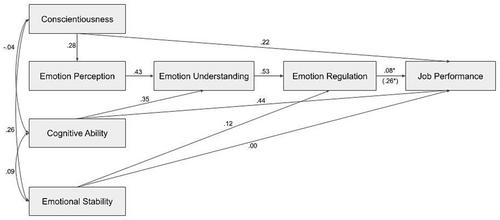
In this article, we demonstrate how developments in the emotional intelligence (EI) field can be applied to the challenge of selecting for, and developing, relevant interpersonal care skills in medical students and physicians. The concept of EI itself has been somewhat controversial. However, a more nuanced understanding of EI has evolved in the light of research findings that can be applied to medical selection and education. Specifically, we propose modifications to the existing ‘cascading’ model of EI. This model identifies, and relates, several key socioemotional skills and traits that could be considered as ‘the elementary particles’ of EI required to deliver compassionate, person-centred care.
Our model of EI, which is relevant to care delivery, identifies putative targets for both medical selection and training. Selection for medical school and subsequent clinical education should focus on screening out those with low levels of the traits and abilities less amenable to training. Conversely, medical education should be concerned with developing and maintaining the socioemotional skills, attitudes and behaviours critical to the delivery of compassionate, person-centred care. This is especially important for specialties characterised by high levels of emotional labour and possible resultant compassion fatigue.