The Interpersonal-Psychological Theory of Suicide proposes that capability for suicide is acquired through exposure to painful and provocative events (PPEs). Although there is robust evidence for a positive association between aggregate measures of PPEs and risk for suicidal behavior, little is known about the contributions of physical injuries. The present study investigated the relationship between injuries and risk of subsequent suicide attempt (SA).
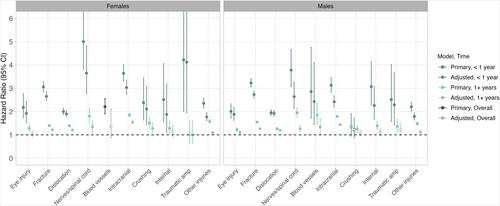
Data were from Swedish population-based registers. All individuals born in Sweden between 1970 and 1990 were included (N = 1,011,725 females and 1,067,709 males). We used Cox regression models to test associations between 10 types of injuries (eye injury; fracture; dislocation/sprain/strain; injury to nerves and spinal cord; injury to blood vessels; intracranial injury; crushing injury; internal injury; traumatic amputation; and other or unspecified injuries) and risk for later SA. Analyses were stratified by sex and adjusted for year of birth and parental education. Additional models tested for differences in the pattern of associations based on age group and genetic liability for SA. In co-relative models, we tested the association between each injury type and risk for SA in relative pairs of varying genetic relatedness to control for unmeasured familial confounders.
All 10 injury types were associated with elevated risk for SA (hazard ratios [HRs] = 1.2–7.0). Associations were stronger in the first year following an injury (HRs = 1.8–7.0), but HRs remained above 1 more than 1 year after injury exposure (HRs = 1.2–2.6). The strength of associations varied across injury type, sex, age, and genetic liability for SA. For example, the magnitude of the association between crushing injury and risk for SA was larger in females than males, whereas other injuries showed a similar pattern of associations across sex. Moreover, there was evidence to support positive additive interaction effects between several injury types and aggregate genetic liability for SA (relative excess risk due to interaction [RERI] = 0.1–0.3), but the majority of these interactions became non-significant or changed direction after accounting for comorbid psychiatric and substance use disorders. In co-relative models, the pattern of associations differed by injury type, such that there was evidence to support a potential causal effect of eye injury, fracture, dislocation/sprain/strain, intracranial injury, and other and unspecified injuries on risk for SA. For the remaining injury types, HRs were not significantly different from 1 in monozygotic twins, which is consistent with confounding by familial factors.
Injuries are associated with increased risk for subsequent SA, particularly in the first year following an injury. While genetic and familial environmental factors may partly explain these associations, there is also evidence to support a potential causal effect of several injury types on future risk for SA.